Berkeleyan
QB3 + Gates’ millions = a cure?
Helped by Microsoft’s founder, Jay Keasling and his industry partners hope to create an inexpensive treatment for malaria
![]()
| 12 January 2005
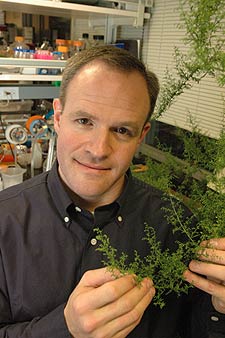 Jay Keasling’s goal is to extract from sweet wormwood the genes involved in the synthesis of artemisinin, then insert them into microbes to build bacterial factories for the drug. (Peg Skorpinski photo) |
And with the announcement last month of a $42.6-million grant from the Bill and Melinda Gates Foundation, that once-illusory goal is closer than ever.
“I’m particularly attracted to research for developing-world problems,” says Keasling, a professor of chemical engineering and bioengineering. “There is so much research funding focused on diseases of the developed world and so little funding for diseases that impact the rest of the world, particularly the poor. Because of the lack of funding, very few researchers are working on these diseases, there is not much competition, and if you find the solutions, you can really make a difference.”
Keasling recently made headlines when he traveled to Samoa to sign a landmark agreement between UC Berkeley and the Samoan people to return to them half of any profits from production of a promising anti-AIDS drug he hopes to produce using similar breakthrough technology.
Now, thanks to the Gates grant, he will seek to create in his laboratory an inexpensive form of the anti-malarial drug, artemisinin —one that he says could be sold for one-tenth of today’s price. That’s 21 cents, about the price of chloroquine, the former frontline anti-malarial that now is meeting resistant strains of the disease around the world.
| A quarter a course to save millions of lives? A $42.6-million grant from the Bill and Melinda Gates Foundation to the Institute for OneWorld Health, the first nonprofit pharmaceutical company in the U.S., will create a powerful new approach to developing a more affordable, accessible cure for malaria, which kills more than a million children each year. OneWorld Health, which announced the grant last month, will work in partnership with UC Berkeley and Amyris Biotechnologies. Berkeley will conduct research to perfect a microbial factory for the compound artemisinin, currently the most effective treatment for malaria, and Amyris, a new biotech company founded on the breakthroughs in synthetic biology pioneered at Berkeley, will develop the process for industrial fermentation and commercialization. OneWorld Health will perform the drug-development and regulatory work to demonstrate the bioequivalence of microbially produced artemisinin derivative to the drug’s natural form. Malaria has become increasingly resistant to frontline medications, but combination drugs containing artemisinin show nearly 100-percent effectiveness after a three-day regimen. But at $2.40 per adult course, these drugs are still beyond the reach of millions of the world’s poorest people. Each year, as many as a half-million people become infected with malaria, and at least 1.5 million die, primarily children in Africa and Asia. The new partnership will utilize a high-technology solution to bring down the cost of treatment to between 20 and 30 cents per course, a more affordable price for patients in developing countries. “This is an extraordinary partnership between public and private institutions that combines cutting-edge science with a commitment to affordability and accessibility for those people in need,” said Regina Rabinovich, director of infectious diseases at the Gates Foundation. “I hope that UC Berkeley’s participation will serve as a model for other academic institutions to apply their scientific knowledge and resources to critical global health problems.” — R.S. |
The artemisinin project is “a great example of QB3 in action,” Keasling says. “We’re taking a natural product in short supply, using biotechnology to produce it and to [do so] very inexpensively in the Third World. It is a real motivation for graduate students and postdocs working at the bench with day-to-day details, knowing that their research will be applied to saving millions of lives.”
A pioneer in synthetic biology
Raised on his family’s corn, soybean, and cattle farm outside Lincoln, Neb., Keasling attended nearby University of Nebraska. There he developed an early interest in microbiology that he went on to pursue through a Ph.D. in chemical engineering from the University of Michigan and a one-year postdoctoral stint at Stanford.
By the time he arrived at Berkeley’s Department of Chemical Engineering in 1992, he had a hybrid background of chemical engineering and biochemistry, and novel ideas about how to re-engineer enzyme reactions in microbes.
At the time, chemical engineering was moving beyond the petrochemical industry into biotechnology, where bacteria were being adapted as chemical factories. Keasling was at the forefront of an area now dubbed “synthetic biology.”
“Chemical engineers are good at integrating lots of pieces together to make a large-scale chemical plant,” he says, “and that is what we’re doing in modern biological engineering: taking lots of little genetic pieces and putting them together to make a whole system. Really, we are designing the cell to be a chemical factory. We’re building the modern chemical factories of the future.”
In 2003, at Lawrence Berkeley National Laboratory, he was appointed head of the first synthetic-biology department in the country, and he’s also working to build a synthetic-biology center at Berkeley. His lab work already has resulted in engineered bacteria that clean up toxic waste, including heavy-metal contamination, and he’s trying to create a bug that feeds on nerve agents and organophosphate pesticides.
To Keasling, the advantage of creating chemical factories inside bacteria is not solely a less expensive product, but also a more environmentally friendly production process. Traditional synthetic chemistry inherently produces toxic waste products — the solvents and reagents typically used in chemical reactions. In addition, extraction from plants risks environmental destruction, especially if it requires the harvesting of rare plants from the wild. A complete chemical factory inside a living cell avoids both these problems.
Besides artemisinin, Keasling plans to make, for example, the anti-cancer drug taxol, a product of the Pacific yew tree, by tweaking the bacterial factory he already has. He also intends to produce Prostratin, the promising anti-AIDS drug first isolated from the native mamala tree in Samoa.
“I think there is a culture here — you see it in the undergraduates and the graduate students — of trying to do something more than just make a lot of money or get a degree,” Keasling says, explaining why it makes sense to be working at Berkeley. “It’s about trying to do something in an area where it will help people.”
A mission to help
The need for an inexpensive version of artemisinin was brought home to Keasling and the pharmaceutical industry shortly after the World Health Organization and other global donors jointly urged nations to adopt artemisinin-like drug combinations as the preferred treatment for malaria. Not long after that April 2004 announcement, drug companies, which make a combination drug treatment from the wormwood plant, began to hear of Asian speculators who were buying up the plant and hoarding it. According to a recent New York Times article, the price of the plant has quadrupled, driving up the cost of the drug and making it even less accessible to the world’s poor, who need it most.
“I’m looking at our timeline, thinking, is there any way we can speed this up?” says Keasling, referring to what he envisions as a five-year program in his lab to bring his bacteria-derived artemisinin drug to Food and Drug Administration approval.
The Gates Foundation, he says, “is performing a unique role in supplying the development costs for this drug so we can offer it to the people in the developing world at cost. Our goal is to make the most effective drug available today — artemisinin — as inexpensive as the drugs that are no longer effective.”

